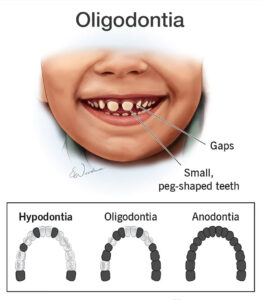
The congenital absence of many, but not all, teeth is known as:
• hypodontia
• oligodontia
• diphyodontia
• anodontia
Answer Key : oligodontia
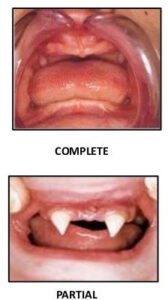
 1. Complete true: is a rare condition in which all of the teeth are missing. It may involve both the primary and permanent dentitions. It is usually associated with hereditary
1. Complete true: is a rare condition in which all of the teeth are missing. It may involve both the primary and permanent dentitions. It is usually associated with hereditaryNote: As a general rule, if only one or a few teeth are missing, the absent tooth will be the most distal tooth of any given type (if molar, then it would be the third molar).
Which type of dentinogenesis imperfecta features multiple pulp exposures, periapical radiolucencies, and a variable radiographic appearance?
• Type I
• Type II
• Type II
Answer Key: Type III
Dentinogenesis imperfecta is an autosomal dominant condition in which there is an intrinsic alteration in the dentin. It affects dentin of both the primary and the permanent dentition. It is also known as hereditary opalescent dentin. Dentinogenesis imperfecta has been subdivided into three types:
• Type I: dentin abnormality occurs in patients that have osteogenesis imperfecta (characterized by blue sclera or a history of bone fractures). In this form, primary teeth are more
severely affected than permanent teeth.
• Type II : most common, only the dentin abnormality exists with no bone involvement.
• Type III (Brandywine Type) like Type II, only the dentin abnormality exists, however, there are clinical and radiographic variations in this type. Features of type III that are not
seen in type I and II include multiple pulp exposures, periapical radiolucencies, and a variable radiographic appearance
Important: Clinically, dentinogenesis imperfecta is usually easily detected and identified. The teeth exhibit an unusual translucent or opalescent appearance with color variation from
yellow-brown to gray. The entire crown appears discolored owing to the abnormal underlying dentin.
Other characteristics of the teeth include:
• Although the enamel is structurally and chemically normal, it fractures easily, resulting in rapid wear (due to poor dentin support)
• There is excessive constriction at the CEJ, giving the crowns a tulip or bell shape
• Short roots
• Obliterated pulps (Type I and 11 only)
*** Note: In Type III, the dentin appears thin, and the pulp chambers and root canal are extremely large, giving the appearance of thin dentin shells.
Treatment is full crown coverage for cosmetic purposes.
Note: These teeth should not be used as abutments because the roots are prone to fracture under stress.
The permanent maxillary centrals in the x-ray below are vital. What is the most probable interpretation of the condition illustrated?
• mesiodens
• concrescence
• fusion
• dens in dente
Answer Key : premolars
Hypercementosis
It is often confined to the apical half of the root but, in some instances, may involve the entire root.
In most instances, it affects vital teeth, is not associated with any one particular systemic disease and may be regarded as a dental anomaly.
It may be seen when a tooth has lost its antagonist or when there is chronic inflammation of the tooth.
The premolars are most frequently involved. Next in frequency are the first and second molars.
Hypercementosis produces no significant clinical signs or symptoms indicative of its presence.
It is seen radiographically as a bulbous enlargement that has, surrounding it, a continuous and unbroken periodontal membrane space and a normal lamina dura.
An enamel defect resulting from the incomplete formation of the enamel matrix is called:
• enamel pearls
• enamel hypocalcification
• enamel hypoplasia
• regional odontodysplasia
Answer Key : enamel hypoplasia
Enamel hypoplasia
It is a developmental defect in which the enamel of the teeth is hard in context but thin and deficient in amount. It results from incomplete formation of the enamel matrix with a deficiency in the cementing substance. Enamel hypoplasia affects both the deciduous and permanent teeth. It is usually due to illness or injury during tooth formation or due to a genetic disorder.
Note: The genetic forms of enamel hypoplasia are generally considered to be types of amelogenesis imperfecta.
The Clinical appearance of enamel hypoplasia includes:
1) the lack of contact between teeth,
2) the rapid breakdown of occlusal surfaces, and
3) a yellowish-brown stain that appears where the dentin is exposed.
The abnormal loss of tooth structure due to nonmasticatory physical friction is referred to as:
• erosion
• abfraction
• attrition
• abrasion
Answer Key : abrasion
Types of abrasion:
1. Toothbrush abrasion: most often results in V-shaped wedges at the cervical margin in the canine and premolar areas. It is caused by the use of a hard toothbrush and/or a horizontal brushing stroke and/or a gritty dentifrice.
2. Occlusal abrasion: results in flattened cusps on all posterior teeth and worn incisal edges. It results from the chewing or biting of hard foods or objects and chewing tobacco.
• Attrition is the wearing away of enamel and dentin due to the normal function or most commonly, due to the excessive grinding or gritting together of teeth by the patient (referred
to as bruxism). The most noticeable effects of attrition are polished facets, flat incisal edges, discolored surfaces of the teeth, and exposed dentin. Facets usually develop on the linguoincisal surface of the maxillary central incisors, the facioincisal surface of the mandibular canines, and the linguoincisal surface of the maxillary canines.
• Erosion is the loss of tooth structure from nonmechanical means. It can result from drinking acidic liquids or eating acidic foods. It is common in bulimic individuals as a result
of regurgitated stomach acids. It affects smooth and occlusal surfaces.
• Abfraction lesions are cervical erosive lesions that cannot be attributed to any particular cause; causing the enamel to “pop” off starting at the base of the tooth and exposing the gumline of the tooth to excessive wear.
In Type I dentin dysplasia, roots appear extremely short, and pulps are:
• normal
• somewhat smaller
• extremely large
• completely obliterated
Answer Key : completely obliterated
Dentin dysplasia
• Extremely short roots
• Obliterated pulp chambers and root canals before eruption
• Residual fragments of pulp tissue appear typically as horizontal lucencies (chevrons)
• Periapical radiolucencies (granulomas or cysts) around the defective roots
Leukemia is a group of bone marrow diseases involving an uncontrolled increase in:
• red blood cells (erythrocytes)
• platelets
• plasma cells
• white blood cells (leukocytes)
Answer Key : white blood cells (leukocytes)
Leukemia
It is a form of cancer that begins in the blood-forming cells of the bone marrow (the soft, inner part of the bones).
Under normal circumstances, the blood-forming, or hematopoietic, cells of the bone marrow make leukocytes to defend the body against infectious organisms such as
viruses and bacteria.
But if some leukocytes are damaged and remain in an immature form, they become poor infection fighters that multiply excessively and do not die off as they should.
The leukemic cells accumulate and lessen the production of oxygen-carrying red blood cells (erythrocytes), blood-clotting cells (platelets), and normal leukocytes.
If untreated, the surplus leukemic cells overwhelm the bone marrow, enter the bloodstream, and eventually invade other parts of the body, such as the lymph nodes, spleen, liver, and central nervous system (brain, spinal cord).
In this way, the behavior of leukemia is different than that of other cancers, which usually begin in major organs and ultimately spread to the bone marrow.
There are more than a dozen varieties of leukemia, but the following four types are the most common:
1.Acute lymphocytic leukemia (ALL): most common type in children
2. Acute myelogenous leukemia (AML): most malignant type
3. Chronic lymphocytic leukemia (CLL): least malignant type
4. Chronic myelogenous leukemia (CML): 2 distinct phases, invariably fatal
Important:
• Leukemia is classified by the dominant cell type and by the duration from onset to death
• Leukemia can modify the inflammatory reaction
• Leukemia’s effect on teeth/gingiva: Due to a decrease in immune response, periodontal problems can be aggravated. Gingival enlargement can be a finding with leukemia. Additionally, deficits with platelets can be seen intraorally with increased hemorrhaging/bruising.

Enter your email address to receive our Free Newsletter for key Exam and Resource Updates